If you prefer videos, make sure to watch the video above as we discuss all the essential dentistry diagnoses with lots of photos to help!
In this blog we cover all the essential Dental Diagnoses you need to know including caries, pulpal, periapical. periodontitis (gum disease), tooth surface loss (Erosion, Attrition, Abrasion, Abfraction), dentine hypersensitivity and some others!
Caries
The first diagnosis we’re going to be covering is caries. There are loads of different ways of diagnosing caries but the main ones that you’re going to use are visual, tactile and radiographic. Caries can start as an active white spot lesion and these look smooth, frosty, opaque and non-cavitated and are detected more easily when air dried for a few seconds with a 3in1 syringe. As the caries progresses, they become roughened, chalky and microcavitated and now you can detect them by running probe along the surface. There are no symptoms at this stage and if the plaque is removed, the lesion can arrest and become a brown spot lesion with a hard shiny surface.
Pulpal and Periapical
Caries progresses into dentine without much lateral spread, but once it reaches the Enamel Dentine Junction, it spreads laterally along this junction and down the dentine tubules towards the pulp. And this is where the patient might start getting some symptoms of reversible pulpitis. The standout symptoms are a localised, sharp pain, which lasts a few seconds, and comes on when the patient has something hot, cold or sweet. And it’s called reversible because if you treat the caries by doing a filling, the pulp should return back to its normal healthy state and stop causing symptoms.
If the caries is not treated, it will approach the pulp and cause it to become chronically inflamed. At this stage it is called symptomatic irreversible pulpitis with symptoms of a spontaneous, dull, and prolonged pain that last several minutes. It is irreversible because if we just remove the caries and do a filling, the pulp will remain inflamed and cause pain and so there is a need for a root canal treatment.
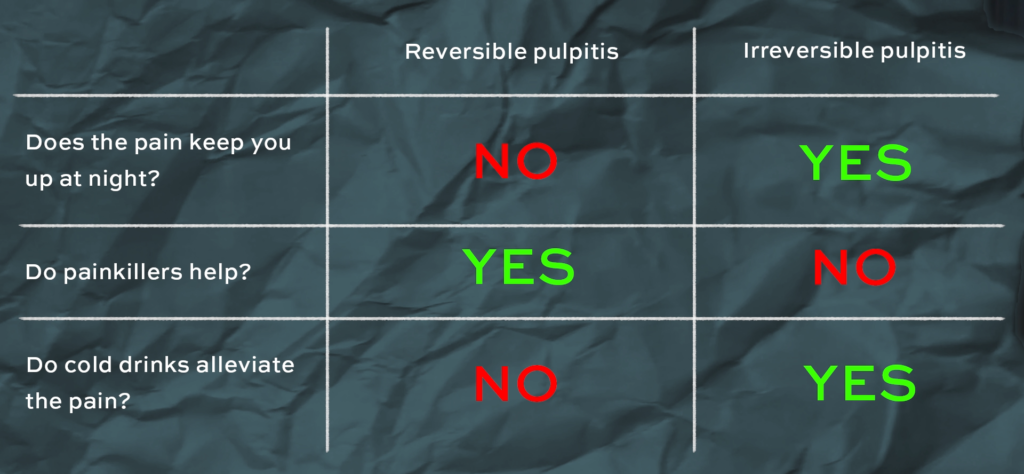
Other than the presentation of the pain, there are a few questions you can ask your patient to differentiate between reversible and irreversible pulpitis:
- Does the pain keep you up at night?
- Reversible pulpitis = No
- Irreversible pulpitis = Yes
- Do painkillers help?
- Reversible pulpitis = Yes
- Irreversible pulpitis = No
- Do cold drinks alleviate the pain?
- Reversible pulpitis = No
- Irreversible pulpitis = Yes
Sometimes you might see a patient with a large carious lesion that’s already reached the pulp but the patient doesn’t experience any pain with hot or cold stimuli. This is known as asymptomatic irreversible pulpitis.
Now as the infection advances, the pulp will start to die. This is called pulp necrosis and at this stage the patient may often present with a history of pulpotic symptoms which they no longer have. This as you can imagine is because the nerve endings in the pulp are dead.
So while the pulp is dying, the bacteria will also travels to the periapical tissues and cause symptomatic apical periodontitis or as some others call it acute apical periodontitis. At this stage they get a well localised pain when biting. This is because the periodontal ligament is inflamed, and biting stimulates the pain and pressure sensitive fibres in this area. The bacteria in the necrotic pulp will also leach toxins through the apex, causing a chronic inflammatory response, which leads to bone resorption. If enough bone resorption occurs, this will be seen in the radiograph as an apical radiolucency.
Symptomatic apical periodontitis often presents with symptoms of irreversible pulpitis as well because this is all a dynamic process. One disease leads to another and some diseases happen at the same time. So as the pulp is inflamed a person might experience the symptoms of irreversible pulpitis. And now because the PDL is also inflamed, they will also experience periapical symptoms. If left untreated at this stage, the pulp will die, and they will only experience periapical symptoms.
If the symptomatic apical periodontitis is left to progress, this may become an asymptomatic apical periodontitis, AKA Chronic apical periodontitis and this happens because of chronic inflammation and destruction of the periodontium. This would be visible on a radiograph as a much larger well-defined radiolucency and can re-exacerbate to become symptomatic apical periodontitis again or as other call it an Acute exacerbation of Chronic Apical Periodontitis.
At any point from once the infection has gone through the apex, an acute apical abscess can form. This is a pus filled swelling which can cause severe spontaneous pain and extreme tenderness to touch. There’s lots of pain because the abscess is causing a lot of pressure in the area and if the abscess is able to drain, for example through a sinus tract in the gums, the pressure is relived and the patient will experience little or no pain. A draining abscess like this is called a chronic apical abscess. To find out which tooth is causing the abscess, you can put a GP point in the sinus and take a radiograph. The GP will follow the tract and point to the infected tooth.
The next diagnosis is one that is often missed out. If you carry out a root canal treatment, there is a slight chance that the patient may come back to you soon after with severe pain, sometimes described as worse than before and maybe a swelling. This is known as a pheonix abscess and is mainly caused by inadequate cleaning of the root canals. And you should ALWAYS warn your patients of this before you start root canal treatment.
You might have also come across a disease process called condensing osteitis. We’re not going to go into too much detail on this one because it’s a lot rarer. It’s basically a reaction to dental infection but on the radiograph, it looks radio-opaque because instead of bone destruction, there is more bone deposition. It can happen when there is a low degree of virulence from the infection and the hosts healthy immune system triggers a sclerotic reaction.
Now we’ve covered all the pulpal diagnoses which are, Reversible Pulpitis, Symptomatic Irreversible Pulpitis, Asymptomatic Irreversible Pulpitis, Pulpal Necrosis and the periapical diagnoses which are Symptomatic Apical Periodontitis, Asymptomatic Apical Periodontitis, Acute Apical Abscess, Chronic Apical Abscess, Condensing Osteitis. It is important to note that when you provide a diagnosis for a tooth, you have to give both a pulpal diagnosis and a periapical diagnosis for example, pulp necrosis and symptomatic apical periodontitis of the UL6.
Periodontitis
So we’re going to move on to diagnosis gum disease or periodontitis. You first need to do a periodontal screening for every patient that walks through your door. The screening tool used is called a basic periodontal examination. The British society of periodontology have formed an in-depth sheet (LINK) to follow which we will go through here. Keep in mind that this classification is also used internationally. A BPE scores of 0 indicate healthy gums, while 1 and 2 could indicate some level of gingivitis, depending on how much bleeding you estimate to have seen.
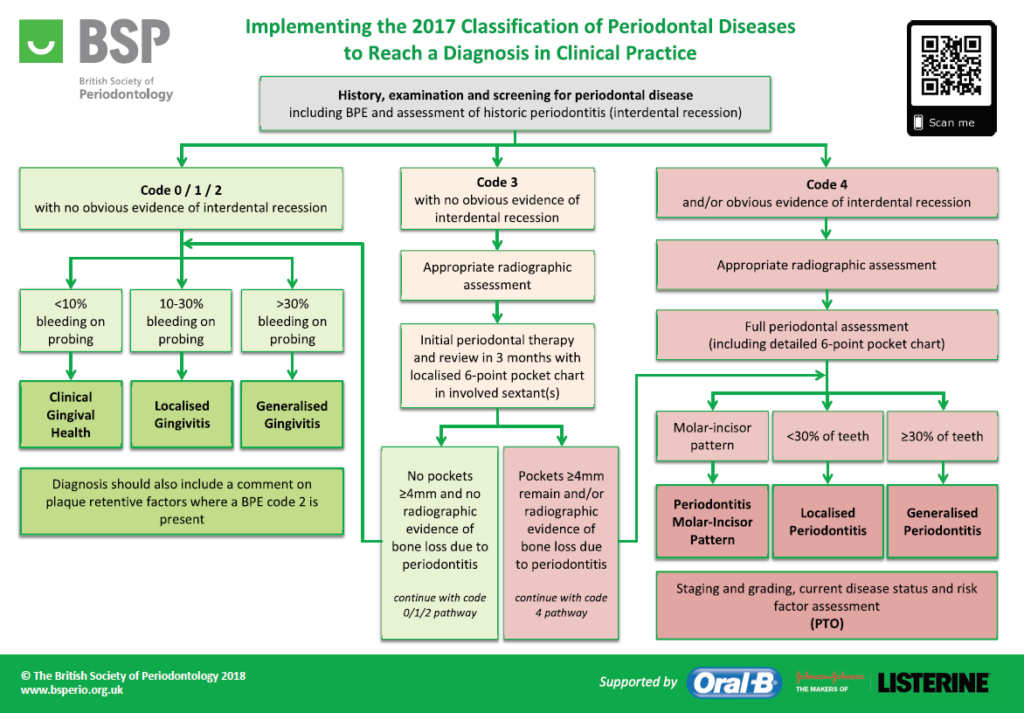
So let’s start by discussing patient who scores 0s and 1s on their BPE. If while you were carrying out your BPE, you saw <10% bleeding when probing, this indicates clinical gingival health. If you saw between 10-30% BOP you will diagnose them with Localised gingivitis and finally if there was more than 30% BOP, this would be Generalised gingivitis. If they also scored a code 2 anywhere, you would supplement the gingival diagnosis with any plaque retentive factors or calculus which might have lead to a 2. E.g.: Localised gingivitis due to overhanging restorations on UR5 UR6.
Now if the patient scores codes 3s or 4s in any sextants then you will need a more in-depth diagnosis consisting of the extent, stage, grade, stability and any associated risk factors. You might not be able to make this full diagnosis on the first appointment and you will understand why in just a moment.
Let’s start with code 3 ONLY, no code 4s. You start by taking radiographs in the sextants with scores of 3 to assess if there has been any bone loss in those areas. You will then do “initial periodontal therapy”, which is just a good supragingival scale and oral hygiene instructions and wait 8-12 weeks for the inflammation to cool down. This will reduce any false pocketing and if it was real pocketing, sometimes just good oral hygiene is enough to close the pocket. Once you have the patient back after 8-12 week, the guidelines say to do a 6 point pocket chart in the involved sextant but we think it’s best if you just redo a BPE, and IF they score a 3 THEN you carry out a 6-point pocket chart of the involved sextants. The 6 point pocket chart will record pocket depth at 6 sites on each tooth, bleeding on probing, mobility, recession, furcation.
So that was for BPE of a 3, but if the first time you saw the patient they had a BPE of 4, you skip the initial periodontal therapy and the 8-12 week wait and you can go straight into taking radiographs, doing a full mouth six point pocket chart and forming your diagnosis.
So now let’s discuss forming your diagnosis. If they had scored 3’s initially but after the initial therapy had no pocket depths ≥4 and no radiographic evidence of bone loss, you can diagnose them using the simpler diagnosis system for BPE’s of 0, 1 and 2. If however you find that they have pocket depths of ≥4 or have bone loss or both, than you proceed to diagnose using the code 4 pathway. And if you’re patient had a BPE of 4 from the beginning, you also diagnose them with this pathway. In this pathway, If you notice that there’s a pattern on just the molars and incisors, this is diagnosed as Periodontitis molar-incisor pattern followed by the staging, grading, stability and risk factors which we will talk about in just a bit. If you find that there is less than 30% of the teeth with pocket depths of ≤4mm and teeth with radiographic evidence of bone loss, this is diagnosed as Localised periodontitis. More than 30% will be Generalised periodontitis.
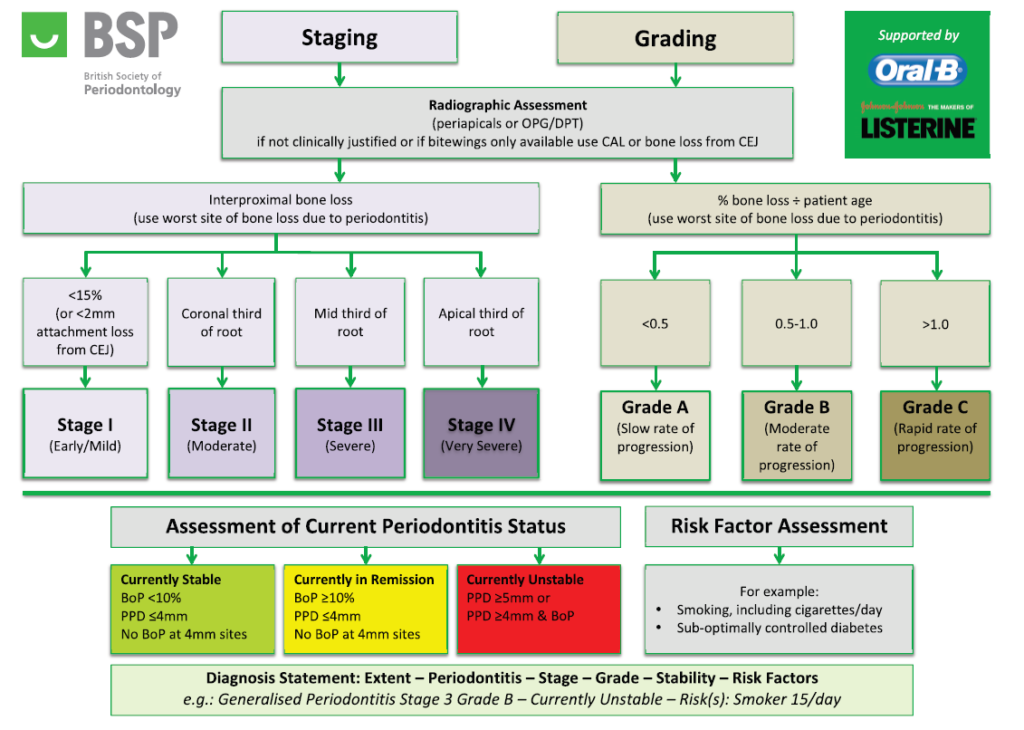
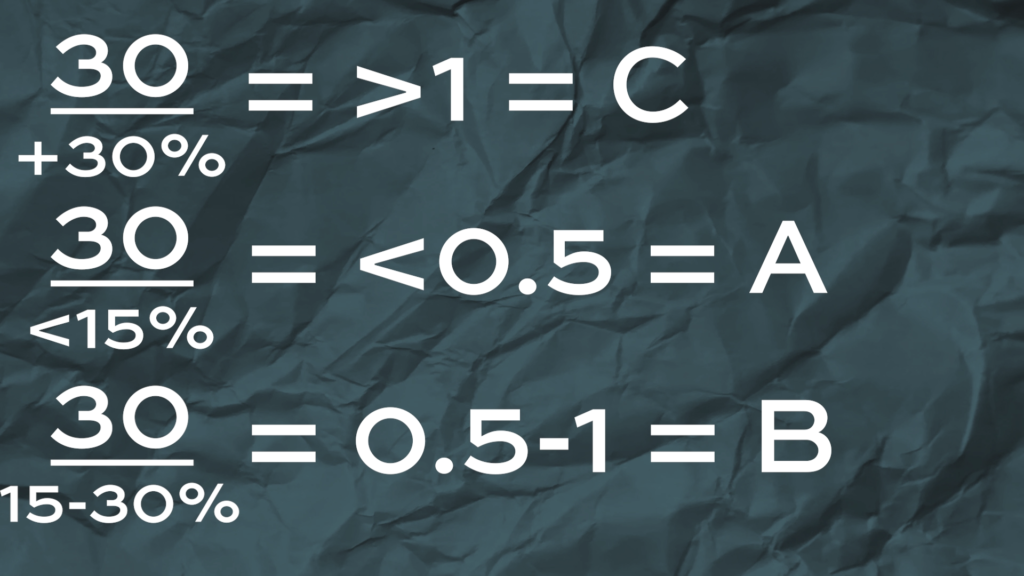
To classify the stage and grade you need the radiograph you took on that first appointment. Staging refers to the severity of the disease and is calculated using the worst site of bone loss while Grading refers to the rate at which the disease is progressing and this is calculated using the percent of bone loss and patient’s age. You don’t actually need to whip out a calculator on clinic by the way, its really simple maths, if the patient is 30 and they have more than 30% bone loss the ratio is >1 which is grade C, and if this same 30 year old had bone loss of 15% this would be a grade A while anything in between is a grade B (see image bellow).
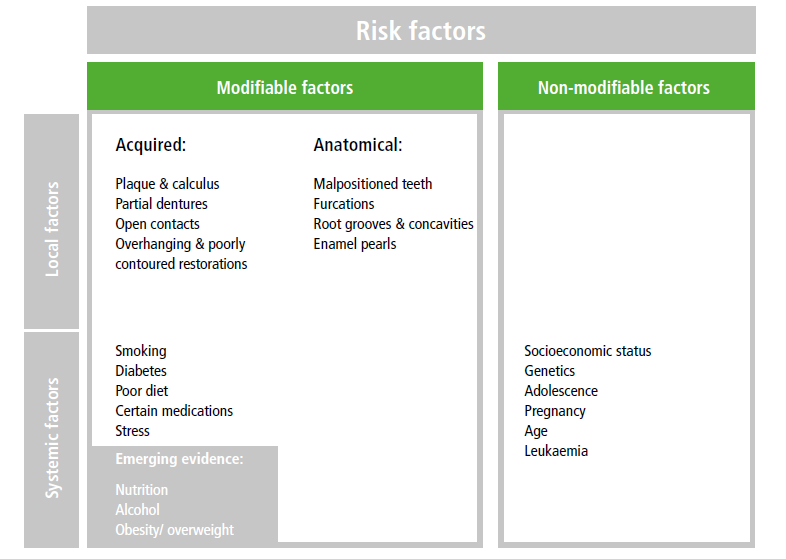
Stability also needs to be assessed and it would be tedious for me to recite to you what you can already read on the guideline but it’s important to note that anything which has a pocket depth of ≥5mm will always be classified as unstable, which is something I’ve heard some of my clinicians arguing is a flaw in the classification because if someone went from having 8mm pockets, down to 5mm pockets, this is an amazing improvement and even if it stays at 5mm for the rest of their lives, it can never be diagnosed as “stable”. Risk factors include things like smoking and diabetes but you look at this full list taken from the full BSP guidelines.
Guide to Periodontology (BSP)
Finally combine everything you’ve found so far and you’ve reached your periodontal diagnosis.
One last diagnosis involving perio that we’ll mention is a lateral periodontal abscess. This is similar to a periapical abscess which we discussed before but the difference is that it’s on the side of the tooth instead of the apex and the pulp is usually vital because pulp necrosis is not the cause here. A periodontal abscess is actually caused by the bacteria inside of a deep periodontal pocket. A pus filled abscess may form when the immune system responds to the bacteria and attempts to isolate the infection from spreading. Usually the pus will drain naturally through the pocket but if there’s something in there blocking the drainage, like caluclus, or trapped food, then the abscess can grow.
Tooth Surface Loss
The next thing we’ll be discussing is tooth surface loss. Tooth surface loss is the loss of hard tissues caused by factors other than caries.
The four types you will see are erosion, attrition, abrasion and abfraction.
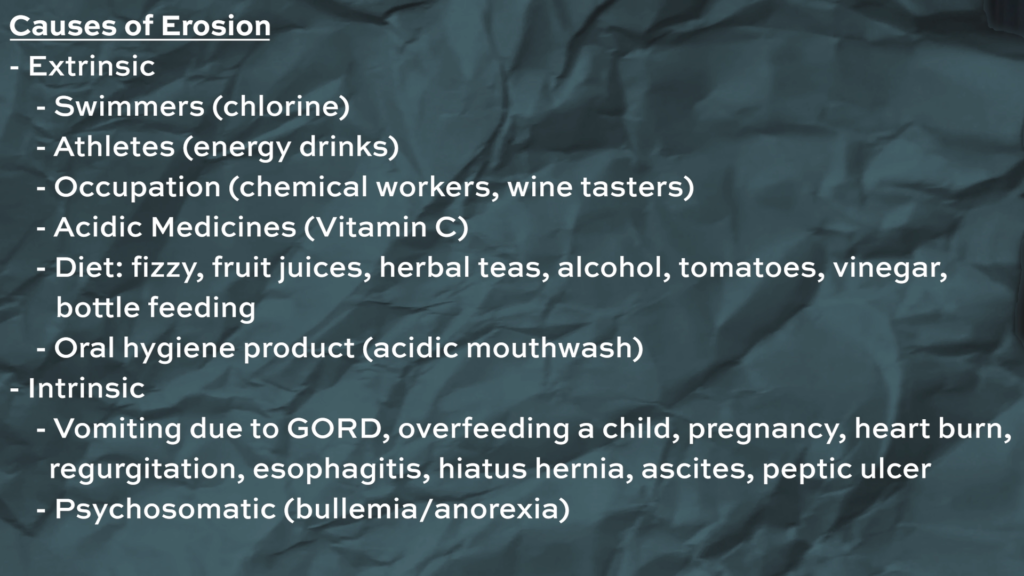
Erosion is Tooth surface Loss caused by a chemical process, like an acid attack, not involving bacteria. And there are both intrinsic and extrinsic sources of acid. Intrinsic sources are things like acid reflux or vomiting. And these patients usually present with palatal tooth surface loss on their upper teeth. With these patients, you don’t see much tsl on the lower molars or incisors because as they have acid reflux or they throw up, the tongue goes over and protects these teeth. Now, Extrinsic sources are mainly diet related, like as fizzy drinks and juices. These patients mostly present with tooth surface loss on the labial surfaces of incisors and occlusal surface of molars. In both types you might see bowl like wear facets, sometimes called a ring of enamel and this happens because the dentine wears away at a faster rate than the enamel. There are also environmental sources of acid like working in environments such as a battery factory. This is a lot rarer now because of stricter health & safety regulations. There are plenty of other causes for erosion, look bellow for the full list that we came up with.
Once you’ve identified the cause, there’s a couple things to look out for when assessing whether or not the Tooth Surface Loss is on-going or arrested. If there’s staining on the teeth, this suggests that it’s been arrested because if it was active, the stained layer would’ve worn out. A sign of inactive Toot Surface Loss is when they used to experience hypersensitivity but now they don’t and when you look into their mouth you can see signs of tooth surface loss like the ones we talked about before. The sensitivity has stopped because the cause of the tooth surface loss has stopped and has allowed time for tertiary dentine to form.
Next type of tooth surface loss is Attrition, which is tooth wear caused by tooth to tooth contact, usually associated with grinding and parafunctional activity. Patients usually present with smooth facets which are flat and match the opposing teeth and you usually see it happening at the same time as erosion. That’s because erosion will demineralise the hard tissues which weakens it and then the grinding wears away the hard tissues. If the TSL by attrition is extensive and rapid, you should expect to see a reduction in the OVD so the patient would look over-closed (or like a grandma with no teeth). You wouldn’t see this if the tooth wear is gradual because dentoalveolar compensation will maintain their OVD. DAC is a process where the alveolar bone remodel’s and elongates to compensate for the loss of VD. For example you can see the differences in the photos bellow. You’ve got no DAC on the left and the gingival margins of all the lower incisors are in one straight line. In the photo on the right you can see the lower incisors are at higher level compared to the canines due to the DAC. You can also see an increased width of the attached gingiva.
Next type of tooth surface loss is Abrasion and it’s tooth wear caused by tooth to non-tooth contact. For example, hard tooth brushing with charcoal activated toothpaste or habits like pen biting. Depending on the habit, the patient will present differently. So for example if a patient is right handed and constantly over brushes the left side of their mouth, you would see this tooth wear on the buccal cervical margins of their upper left teeth. Whereas pen biting can show as chipped incisal edges.
The last type of TSL is known as Abfraction. This is defined as a fracture on the cervical margin which is caused by flexures upon occlusal loading. This is how it looks. Abfraction is sometimes missed out from books which talk about TSL because it’s not believed to be as relevant or necessarily true.
Dentine hypersensitivity
First one on the list is Dentine hypersensitivity and it occurs when there’s exposed dentine and can be caused by things like TSL, trauma, caries, gingival recession and maybe even an over-etched composite filling. The patient would present with a localised, sharp pain to hot, cold and/or sweets. The pain usually only lasts a few seconds and goes away after the stimulus is removed. This pain can be replicated if you blow air from your 3in1 syringe at the tooth but be careful when you do this and make sure you warn the patient before you do, because it can really surprise them.
Cracked tooth syndrome
Another diagnosis you should be aware of is called Cracked tooth syndrome. This is defined as an incomplete fracture in a vital posterior tooth. Your patient might present with a sharp, localised pain which might be made worse by releasing after biting down. The best way to test this is with something called a tooth slooth and there are 2 places you should test, the fissures and each individual cusps. The way you use it is by placing the pointy end on the tooth in question and asking the patient to bite and hold, then release and ask them at what point it hurt them.
Pericoronititis
Second to last on the list is Pericoronitis, which is the inflammation of the operculum, which is the soft tissue surrounding an impacted tooth. You’ll pretty much only see this on 8’s but it can technically happen to any other partially erupted tooth. The patients are usually between 17 and 24 since this is the time when the wisdom teeth erupt, and they present with localised pain, swelling and they might have difficulty opening their mouth. It’s not uncommon to also see lymphadenopathy, bad breath or pus. Sometimes patient come in with a very large swelling and you will need to know if it’s an emergency or not. The signs that would make you consider referring straight to A&E are: Difficulty breathing, difficulty swallowing, or difficulty in sticking their tongue out. Swellings like this in the floor of the mouth can be especially dangerous since they can block the airways and be a cause of death.
Alveolar osteitis (Dry socket)
The last diagnosis we think you should know is called Alveolar osteitis, this is a the fancy way of saying dry socket. It’s the inflammation of the exposed alveolar bone in the socket when a blood clot fails after an extraction. The patient would usually come back 2-5 days post-extraction complaining that they have a severe throbbing pain which is worse now than it was before they had the their tooth removed. They’d also tell you they have bad breath and taste and that’s because food would have been packing into the socket. Blood clots fail by dislodging or never forming in the first place. It can dislodge by the change in air pressure when smoking, using a straw or mouth-washing too aggressively within 24 hours of the extraction. Other risk factors are a difficult extractions, a previous dry socket, diabetes, anti-coagulants or if someone suffers from blood clotting disorders.